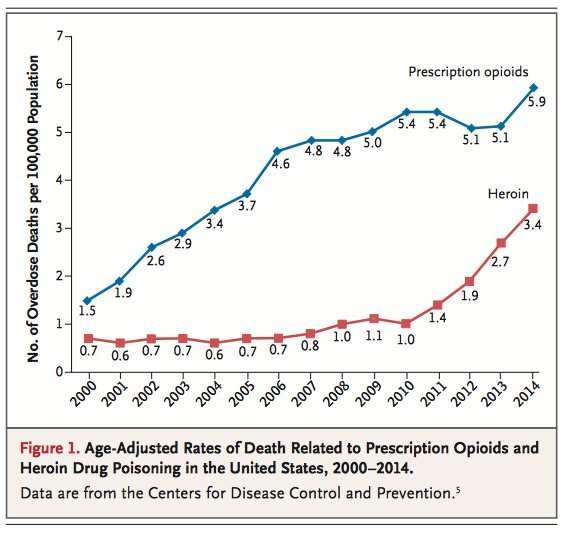
If it seems like you’ve been hearing more and more about the heroin and prescription opioid epidemic (e.g., oxycodone, hydromorphone, morphine, and illicitly made fentanyl) in the news lately, you’re not alone. Over the last several months, this important public health issue has hit the mainstream. HBO ran a special called “Heroin: Cape Cod, USA” that shed light on the addiction problem across the country, focusing on eight families in Cape Cod, Massachusetts. The topic has been mentioned by both Republican and Democratic presidential candidates in debates and town halls. There is even legislation currently making its way through the Senate to address the “opioid-heroin epidemic that is sweeping the country.” This epidemic affects all of us.
Systems thinking
Fighting Moral Decay in Residency
Residency – especially intern year – can be compared to the trenches of war. You are enlisted for a period of time, while you dutifully carry out the orders of superiors, and fight the enemy (disease) while you tend to the already wounded and dying. It removes you from your normal life and can send you into unknown territory, consuming the vast majority of waking hours (sometimes as high as 100-120 hours per week, which is the rarely discussed loophole within the rule of “[no more than] 80 hours per week averaged over a 4-week period”). It can be doubly isolating because the only people who really understand your experience are your compatriots – the co-interns and co-residents fighting in the trenches alongside you. Further, doctors in training, like our veterans, suffer from psychiatric illness and substance abuse issues, but this doesn’t garner much attention unless there is a string of suicides or high-profile articles on the subject. (Time Magazine also ran a story about it in September 2015.) (more…)
Transitions of Care, or Improving Your Health At Home
When explaining the role and importance of public health to my colleagues, I like to jokingly point out that, ideally, patients spend most of their lives outside of the hospital. Though my tone is sarcastic, my sentiment is honest. Most of what happens to people that keeps them healthy or makes them sick happens outside of the hospital setting. One’s habits, lifestyle, home and work environment, level of education, and financial means all influence one’s trajectory of health more strongly than most hospital-based care can. These social, behavioral, and structural determinants of health often make the difference between a person whose health will maintained outside of the hospital and a person who will require repeat hospital visits.
The structural determinant of health that I will discuss in this post is one that I have confronted on a daily basis in the hospital – that of continuity of care, or barriers thereto. The fragmented nature of our healthcare system and the game-of-telephone-like way that information gets passed from one link in the healthcare chain to the next is a major reason that patients’ health and healthcare suffers from systemic discontinuities between hospital, rehab, clinic, and home or facility.
(more…)